
Dr. Martin Edwards uses a baseball and a mitt to demonstrate binding of a Paxlovid component into the active site of the SARS-CoV-2 protease
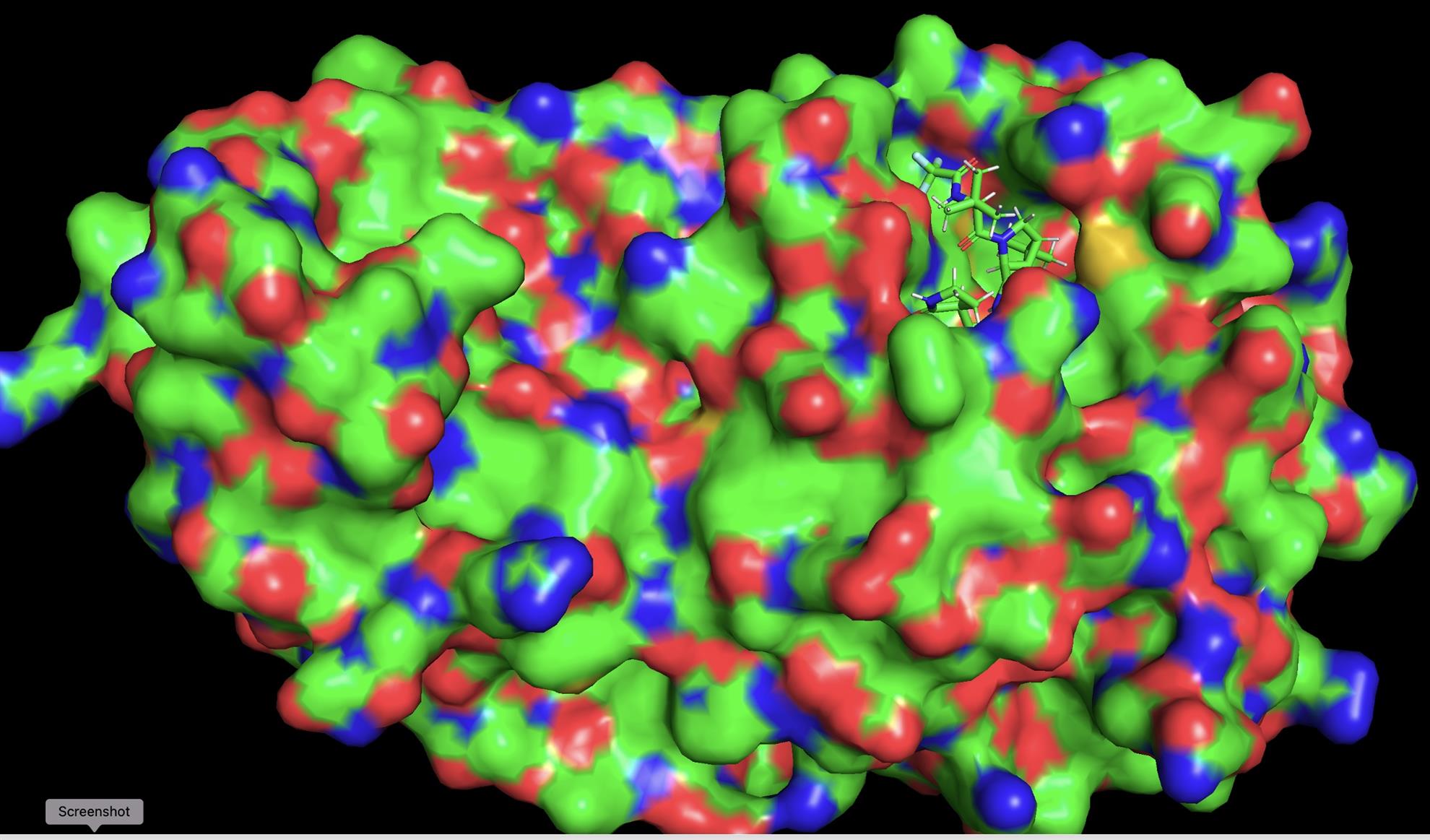
Model of the SARS-CoV-2 protease molecule with the Paxlovid molecule (stick diagram, upper right) blocking the active site (photo courtesy Dr. Martin Edwards)
Dr. Martin Edwards joined our July 28, 2022 meeting to tell the story of how Paxlovid, the treatment for COVID-19 was developed so rapidly. After hearing initial reports from China in January 2020 that a newly-discovered virus could transmit person-to-person, Dr. Edwards thought to himself: “Nearly every person in the world could be infected.” More than half a billion documented infections later, that thought seems to be coming true.
Dr. Edwards said that Paxlovid was propelled by earlier work done on SARS, a virus that is related to SARS-CoV-2, the virus that causes COVID-19, but that failed to cause a global pandemic. Both SARS and SARS-CoV-2 make a protein called a protease that can snip apart different virus proteins so they can assemble to make new viruses that can go on to continue infection, or infect others. Scientists at Pfizer already knew the three-dimensional structure of the SARS protease, and they knew from the SARS-CoV-2 DNA sequence that the SARS-CoV-2 protease would probably have a very similar structure.
Pfizer scientists determined the structure of SARS-CoV-2 using x-ray crystallography, and then analyzed whether molecules in a library containing millions of different chemicals could nestle into a pocket in the protease called the “active site” and block the protease from snipping apart virus proteins. Without the protease snipping, there are no new particles, and infection stops. Dr. Edwards brought a baseball and a glove as an analogy to show how the molecules in Paxlovid fit into the active site pocket. By December 2021, the FDA granted Paxlovid emergency use authorization, and millions of doses have since been administered.
Interested in learning more about the development of Paxlovid and why you might have heard of people “rebounding” (i.e., testing positive after receiving the drug and testing negative)? Check out this NPR story, and articles in JAMA Network and Science.